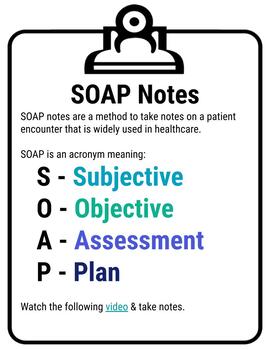
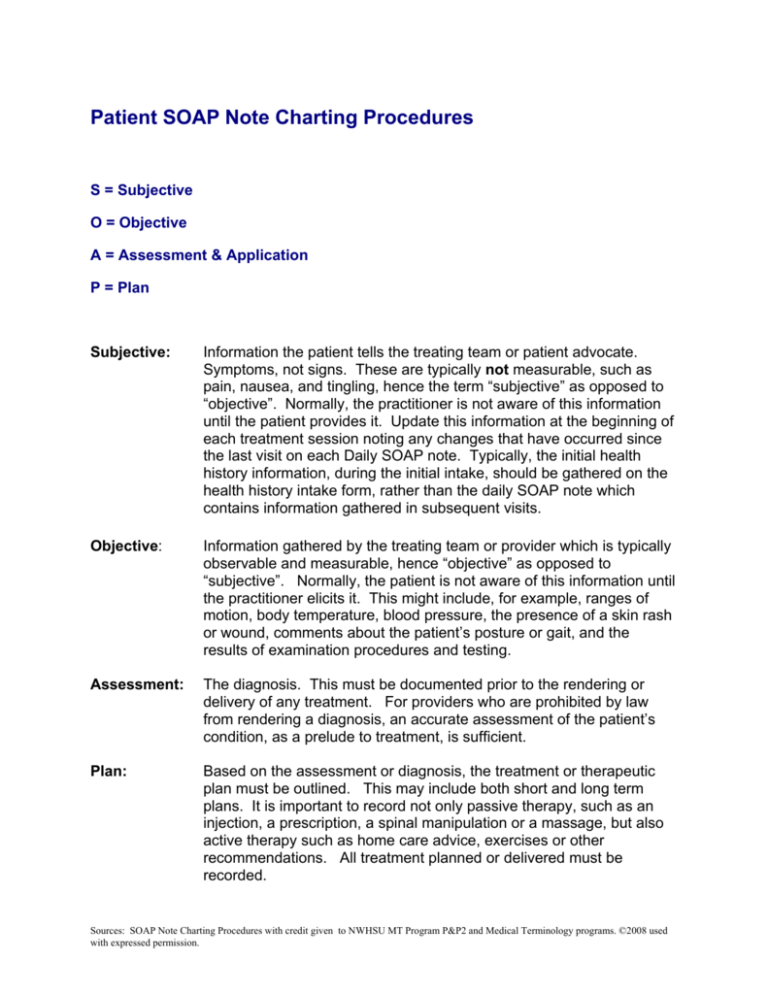
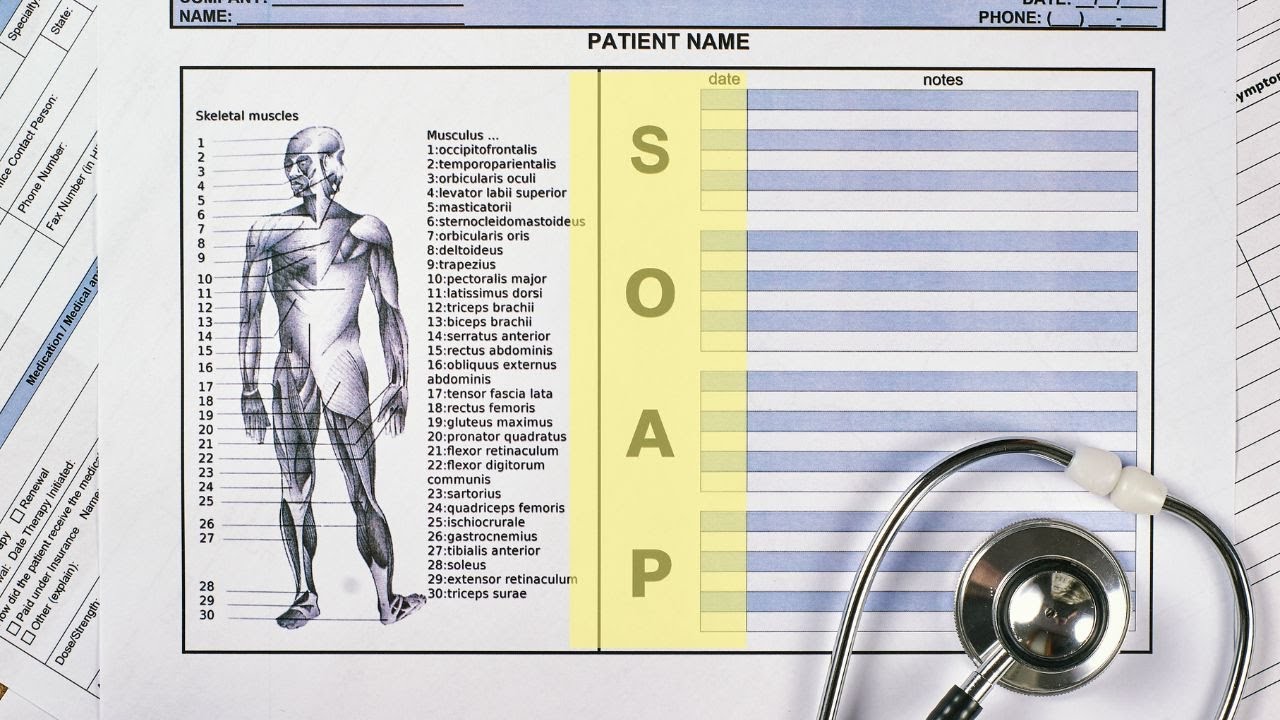
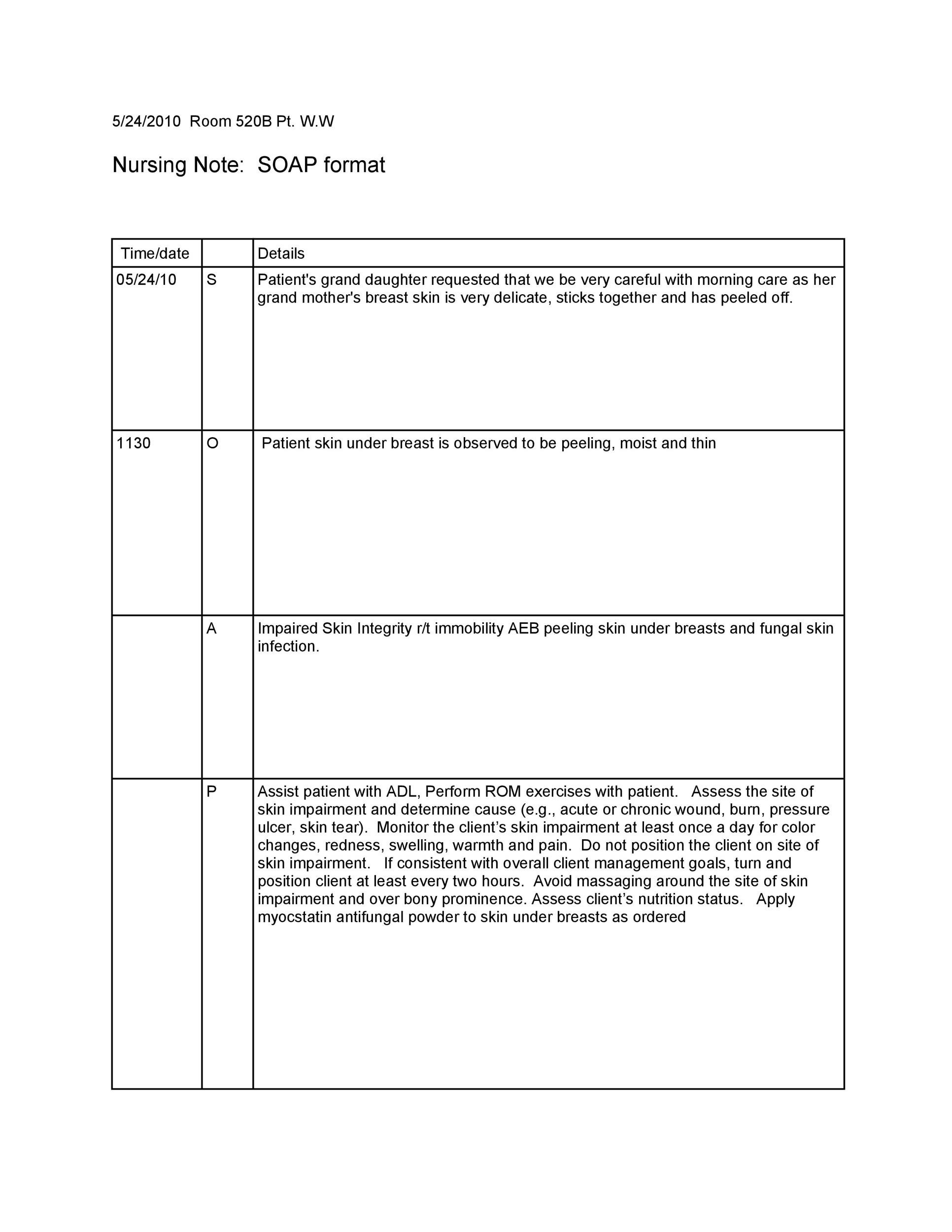
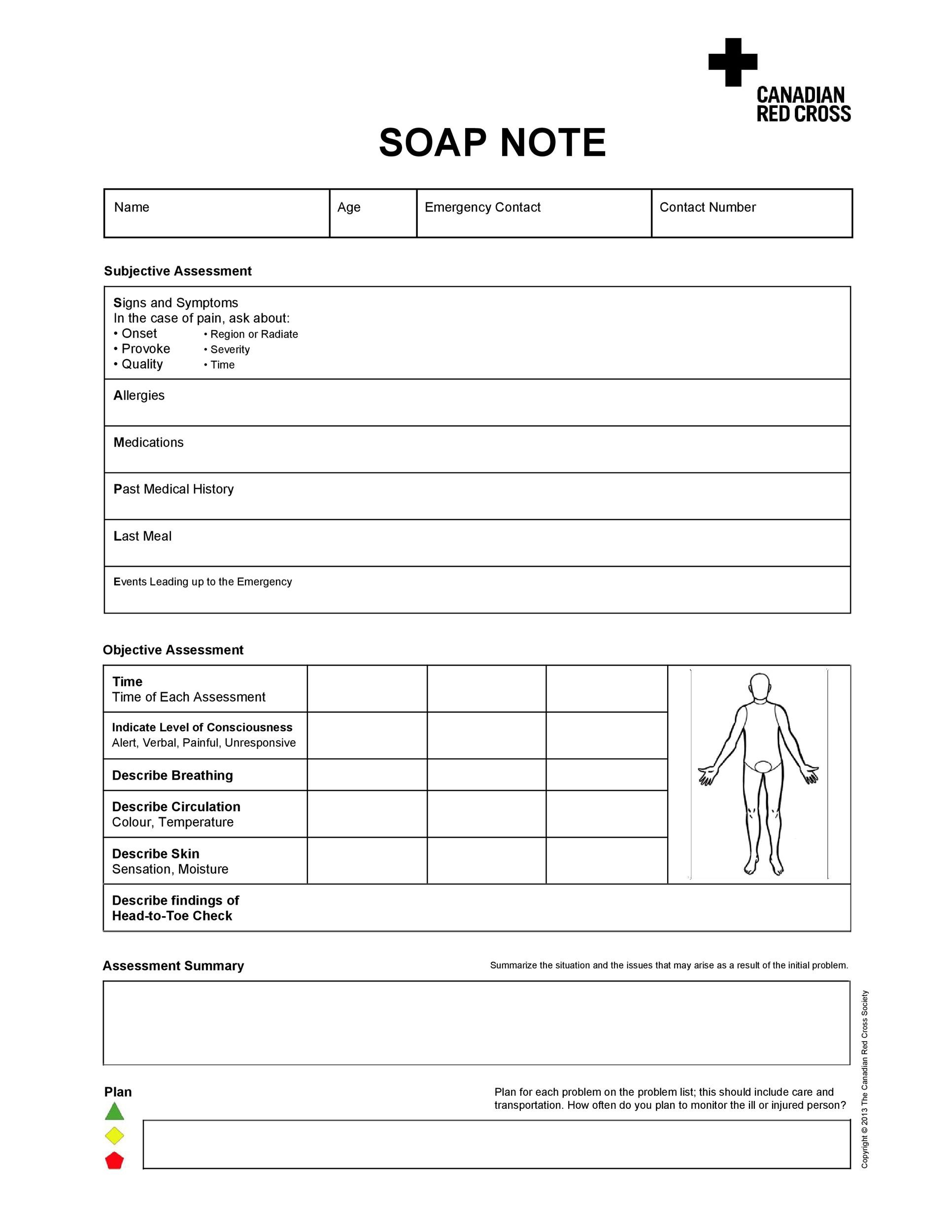
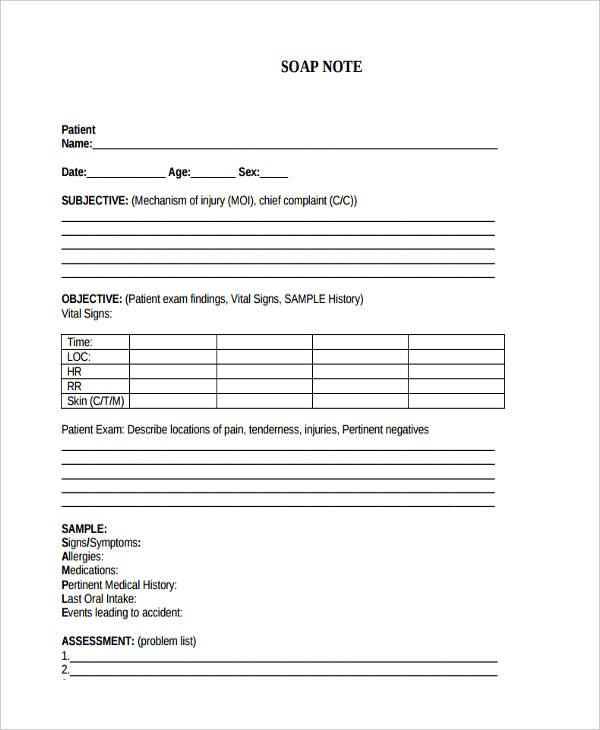
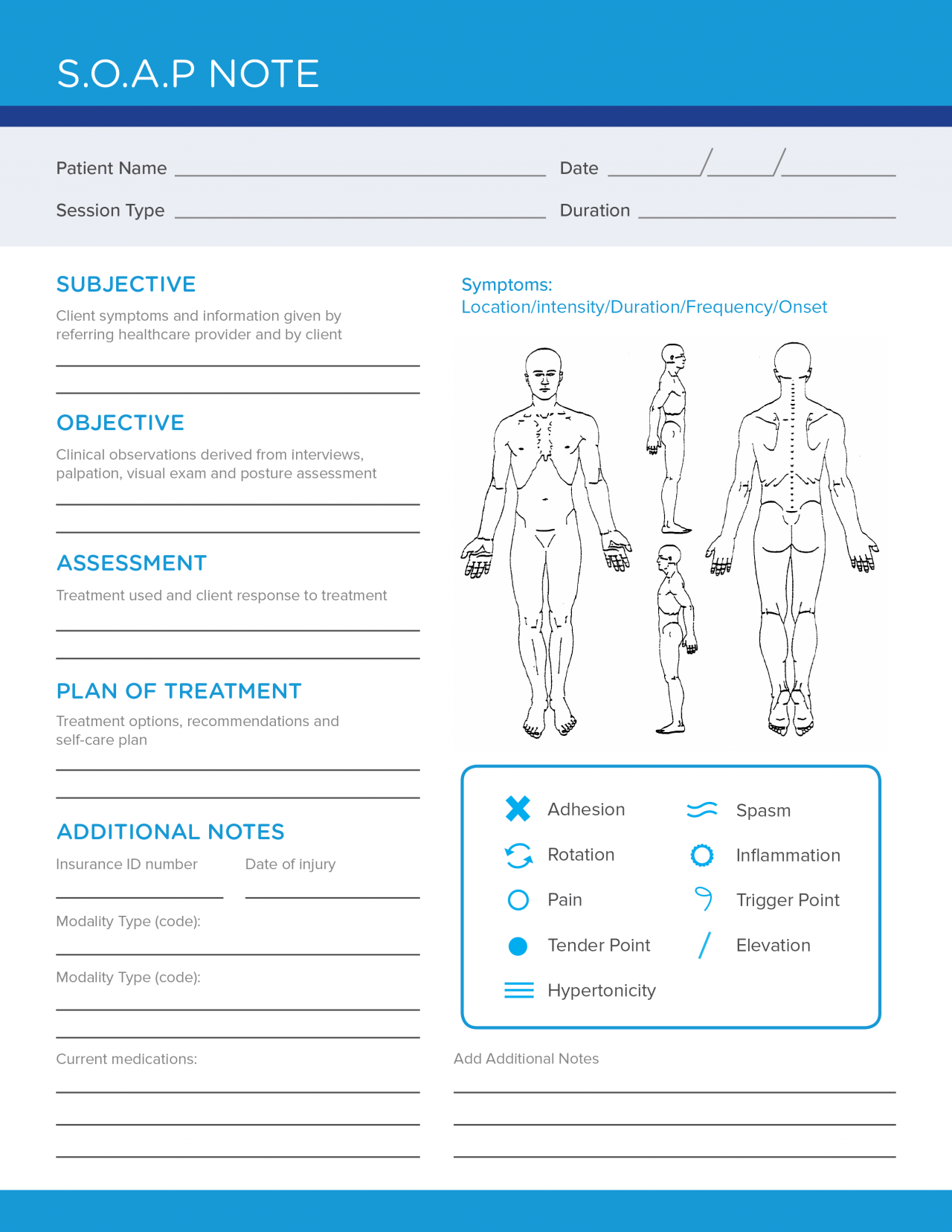
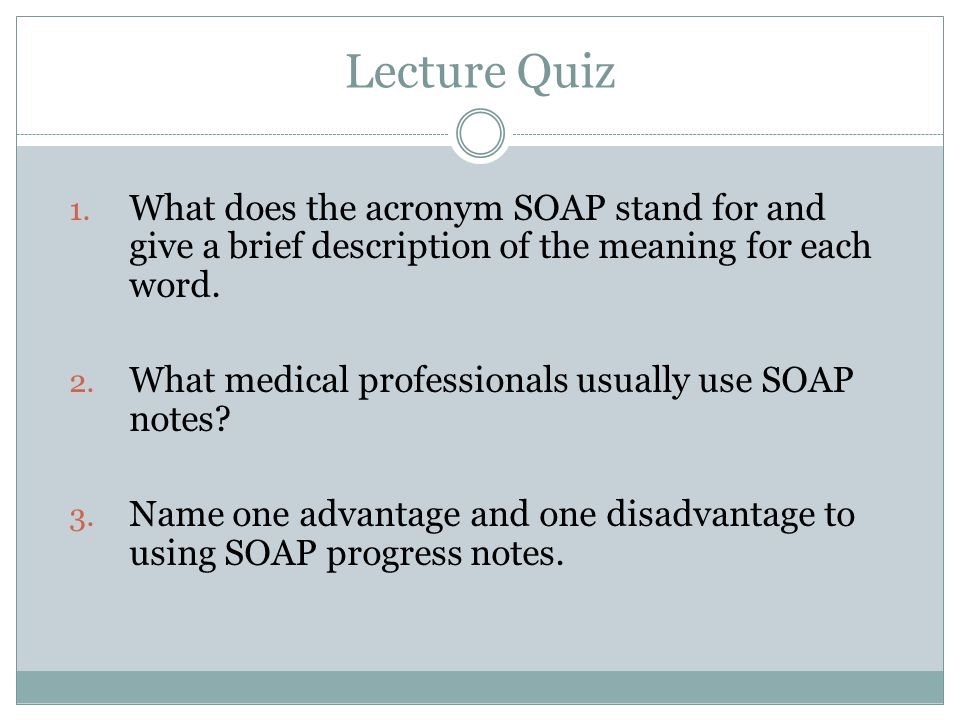
A SOAP note is a document usually used in the medical fraternity to capture a patient's details in the process of treatment This is one of the many formats that The term chiropractic "SOAP notes" has nothing to do with working up a lather So what does "SOAP" stand for?SOAP (an acronym for Subjective, Objective, Assessment, and Plan) is a method of documentation employed by health care providers including massage therapists to write out notes in a patient's chart A Massage Therapist's duty is to assess and treat physical dysfunction and pain of the soft tissue and joints of the body – and SOAP notes
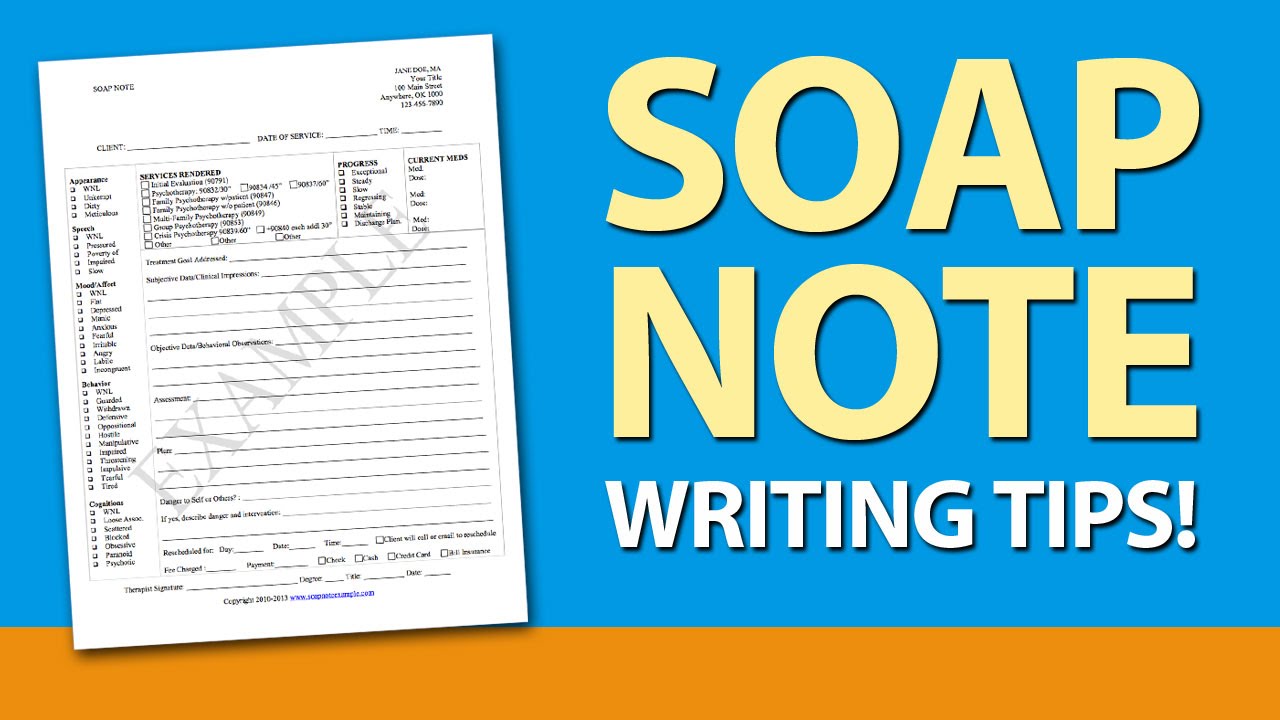
Tips For Writing Better Mental Health Soap Notes Updated 21
What does soap notes mean
What does soap notes mean-List of 3 best SOAP meaning forms based on popularity Most common SOAP abbreviation full forms updated in July 21What does SOAP mean?
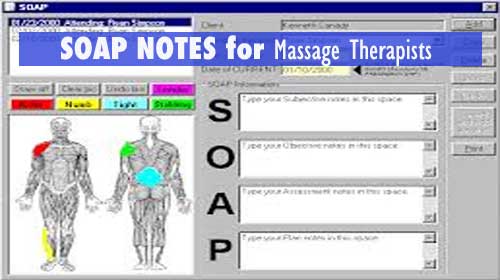



Soap Notes For Massage Therapy
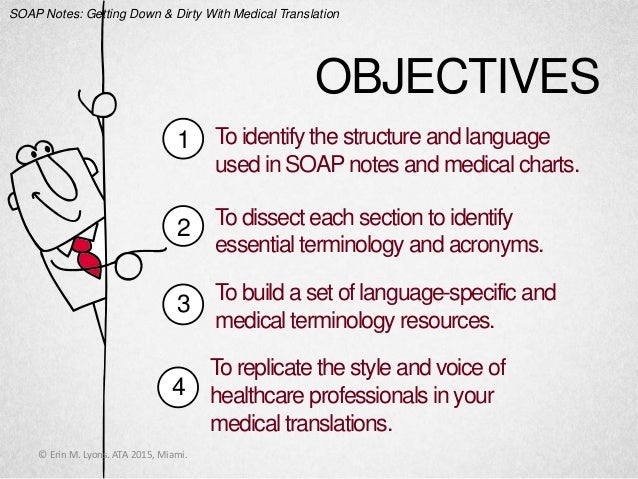
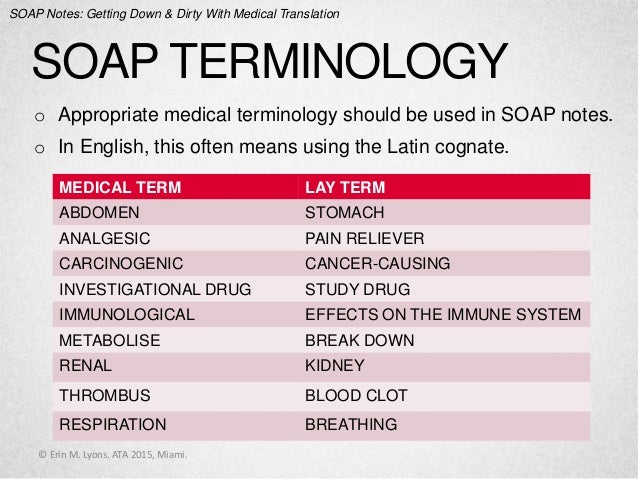
When confronted with a reading passage or document, students need a process to help them begin to determine the purpose or significance of the document It will then be much easier to interpret or even gather evidence from the document when students have a literacy tool to help them begin the processSOAP Simple Object Access Protocol (XML protocol) SoaP Snakes on A Plane (movie) SOAP Standards of Academic Progress SOAP Strategy on a Page SOAP Subjective, Objective, Assessment, Plan (medical documentation format) SOAP Student Opportunity and Access Program SOAP Seal of Approval Process SOAP Spirit of America Party SOAP Society forAssessment New problems / diagnosis identified ;
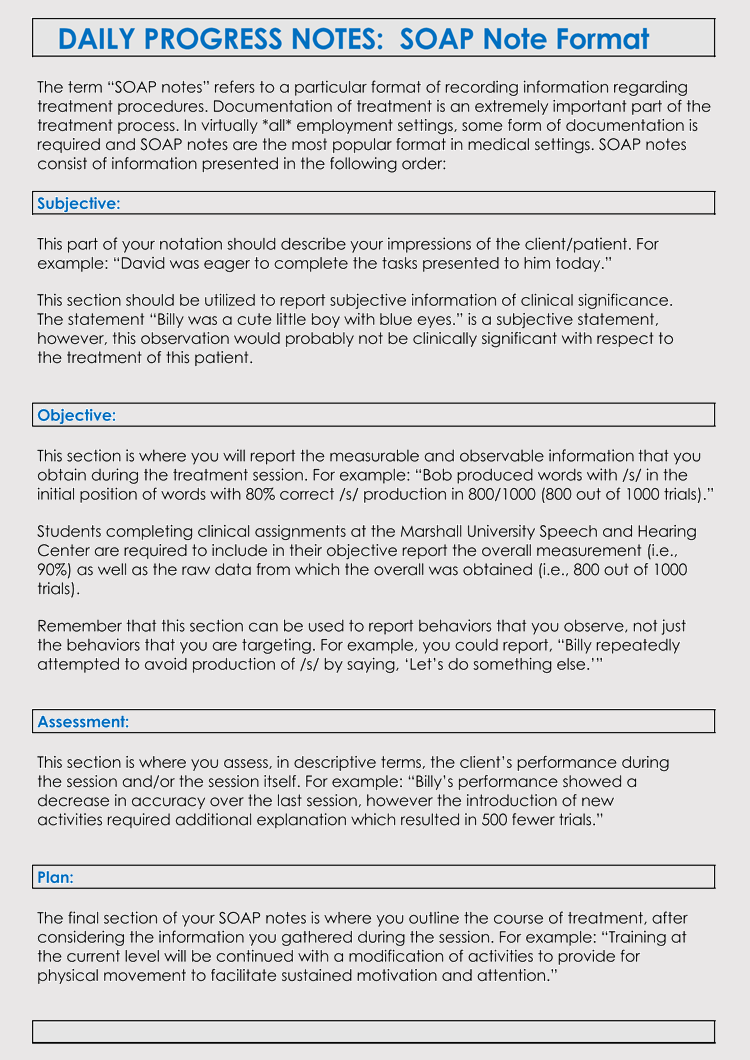
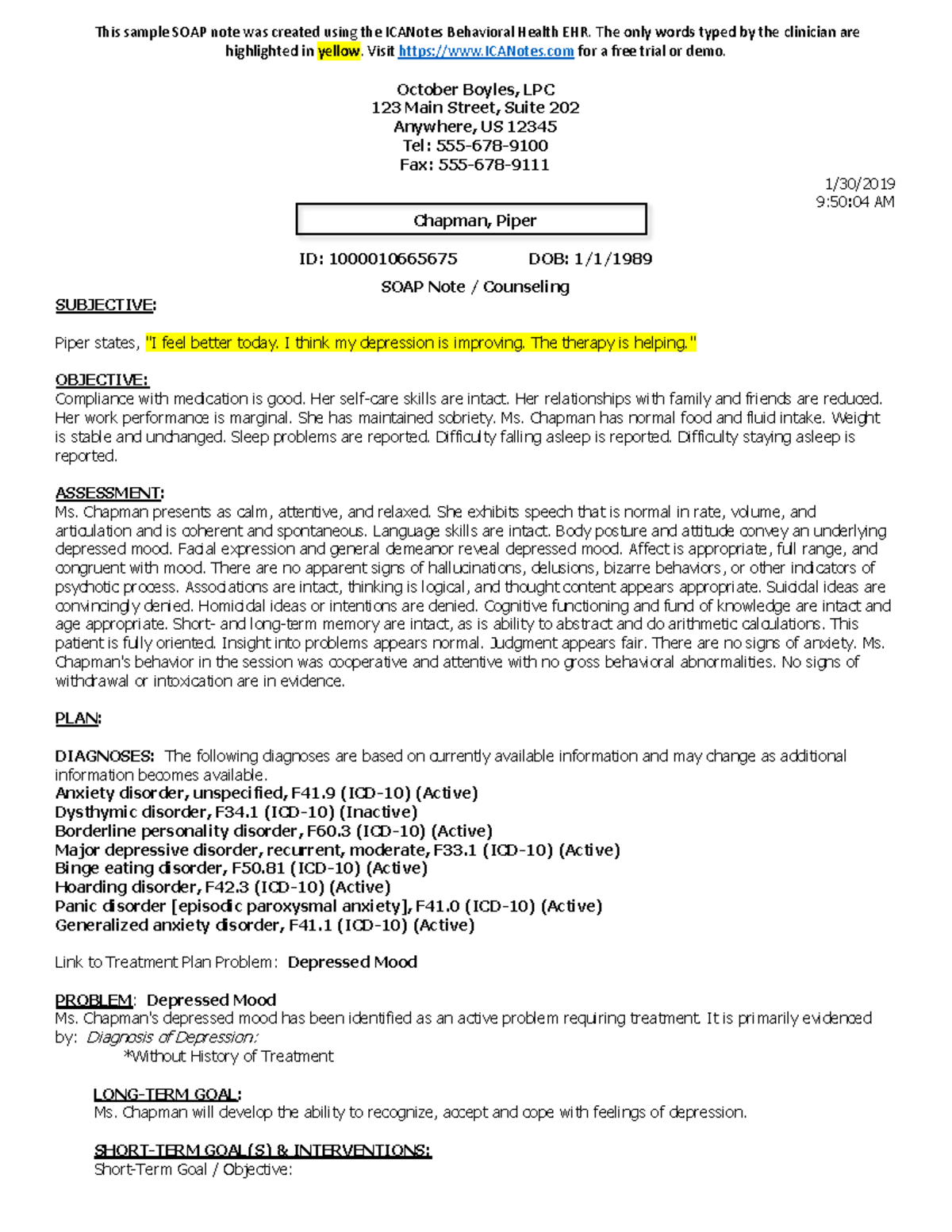
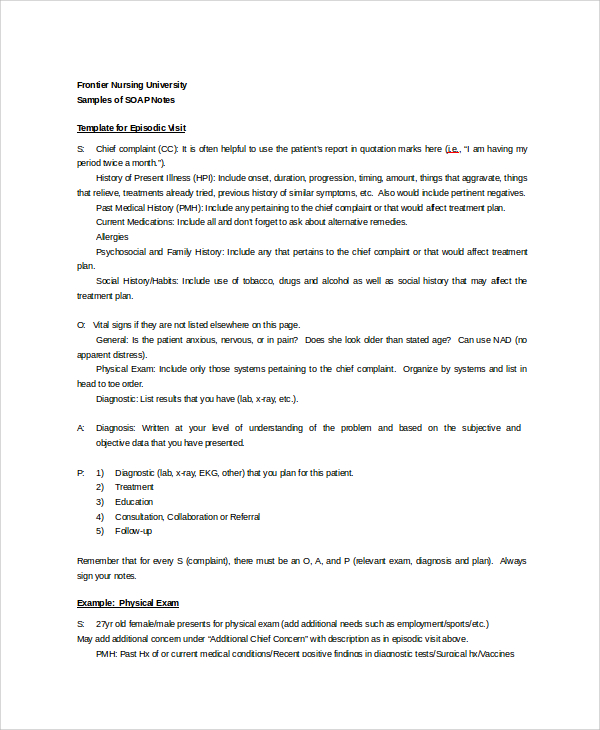
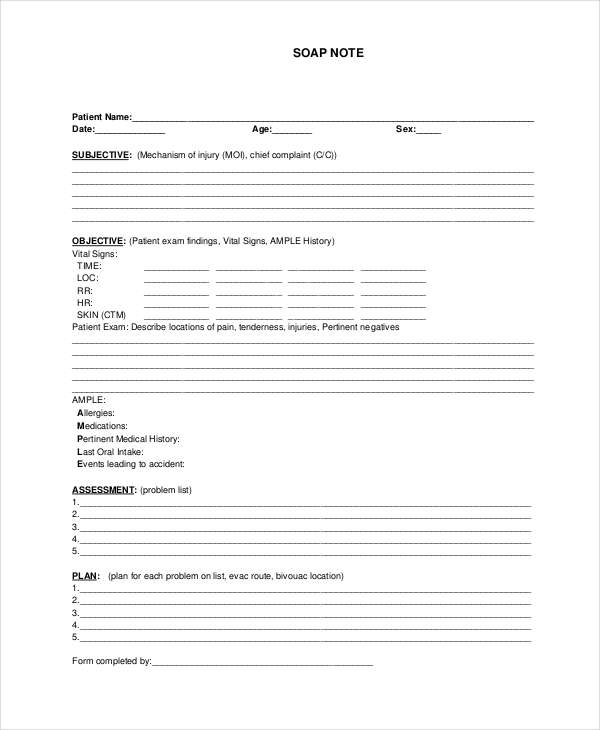
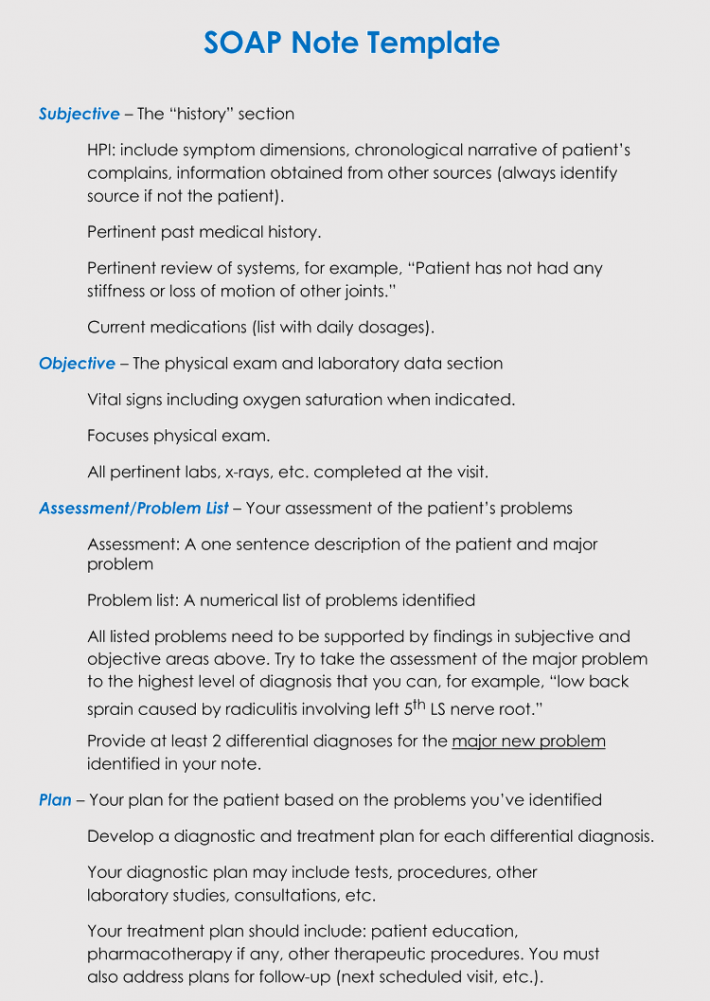
Relevant past medical history;Ongoing problems / issues / diagnosis ; The SOAP note (an acronym for subjective, objective, assessment, and plan) is a method of documentation employed by healthcare providers to write out notes in a patient's chart, along with other common formats, such as the admission note Documenting patient encounters in the medical record is an integral part of practice workflow starting with appointment scheduling,
There are four components that form these notes that make up the acronym SOAP S is for subjective, or what the patients say about their situation It Brian Dear Leave a comment on DAP vs SOAP Notes for Counselors and Therapists Data, Assessment, Plan These are the fundamental building blocks of the DAP note While they serve the same purpose as a SOAP note, DAP is a slightly different format What you choose is entirely up to personal preference The primary thing to keep in mind is that SOAP notes are meant to be detailed, but not lengthy They are a clear and concise record of each interaction with the patient or client Following the format is essential, but it is possible to reorder it so that the assessment and plan appear at the top (APSO)




Soap Note How To Write Spotless Healthcare Notes Free Template Process Street Checklist Workflow And Sop Software




How To Write Incredible Physical Therapist Soap Notes
Acronym for the conceptual device used by clinicians to organize the progress notes in the problemoriented record;Hop on to get the meaning of SOAP acronym / slang / Abbreviation The Medical & Science Acronym / Slang SOAP means AcronymsAndSlang The SOAP acronymSOAP notes include a statement about relevant client behaviors or status (Subjective), observable, quantifiable, and measurable data (Objective), analysis of the information given by the client (Assessment), and an outline of the next course of action (Planning) All SOAP notes should be kept in a client's medical record
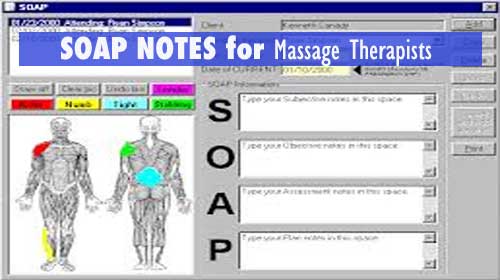



Soap Notes For Massage Therapy



Writing Soap Notes
At the end of Animal Farm, Pilkington and other human farmers come to eat dinner with the pigs at the farmhouse As the other animals watch through the window, they find they are unable to tell pigs and humans apart The pigs have started to dress and behave exactly like humans The book's final image expresses the animals' realization that theO – The O stands for observation what do you see in the verses that you're reading?SOAPS Why use SOAPS when interpreting Primary Source documents?




Note Ets



Counseling Soap Note Example Studocu
SOAP stands for Scripture, Observation, Application, Prayer It's a great way to delve more deeply into your Bible reading, and record your thoughts, emotions and connections when studying scriptureO This is where the SOAPS method can really help to begin creating definitive statements that can be used to evaluate the primary document 2) Writing and Proving Inferences A) Using the information collected in the attention getter, have students write a It is called scientific pitch notation From wikipedia we have Scientific pitch notation (or SPN, also known as American Standard Pitch Notation (ASPN) and International Pitch Notation (IPN))1 is a method of specifying musical pitch by combining a musical note name (with accidental if needed) and a number identifying the pitch's octave So the number is the octave



The Language Of Nursing Notes Mnemonics Notre Dame College Online



Soap Note How To Write Spotless Healthcare Notes Free Template Process Street Checklist Workflow And Sop Software
Spectrometric Oil Analysis Program (SOAP) is a method used by aircraft operators, including several Air Forces of the World, to test the health of aircraft engines by performing frequent laboratory testing of the engine oilThe tests reveal the chemical composition of any metal particles suspended in the oil samples By comparing the results to the known chemical composition ofWho is the audience?Tech Notes What does this mean?




Soap Notes Youtube



Health Science Self Guided Soap Notes Exploration By Laura Miller
Current or persistent symptoms inactive recent problems;Recent test results ; Using SOAP is good medicine Michael H Riegger, DVM, DABVP We all see these articles about what it takes to run a successful practice slick marketing, conflict management, Web pages, team training, appropriate compensation packages, etc The list is endless "You get the best out of others when you give the best of yourself"




What Are Soap Notes In Counseling Examples




Writing Soap Notes Step By Step Examples Templates
S – The S stands for Scripture you physically write out the scriptureyou'll be amazed that what God will reveal to you just by taking the time to slow down and actually write out what you are reading!S stands for subjective data provided by the patient, O for objective data gathered by health care professionals in the clinical setting, A for the assessment of the patient's condition, and P for the plan for the patient's care Here is everything you ever wanted to know about psychotherapy notes definition, difference between SOAP notes, purpose and legal protection 4/9/19 SOAP notes counseling SOAP notes are probably one of the most tedious and confusing things we, therapists and counselors do Review the format and tips on writing SOAP notes in counseling Subscribe to our




Soap Note Flashcards Quizlet
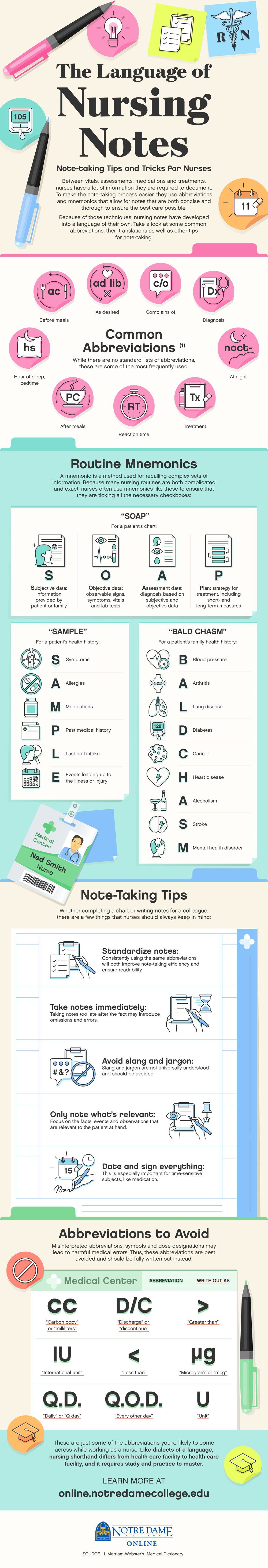



The Language Of Nursing Notes Mnemonics Notre Dame College Online
Taken from Massage Therapy, Principles and Practice, 3rd edition by Susan Salvo Learn with flashcards, games, and more — for freeBeing too brief and concise may mean there is a tendency to over simplify the situation and fail to record what is relevant Deciding what is relevant, is more complicated than simply writing less 'Process recording' ie extensive SOAP notes may lead to writing too much or emphasising unimportant incidents or events Consider the relevance of information recorded, the reasons The term brown note is used when describing a person losing control of their bowels due to sound waves transmitted through the air This theory has yet to be proven




Free Soap Note Templates How To Write Examples Safetyculture




How To Write A Soap Note With Pictures Wikihow
Trading Trade across a variety of markets, whatever your experience level CFD trading, forex trading and bitcoin are all available Find more information under each trading type, including the tools available, costs and charges, strategies, news and analysisPlan notes north enlarged boiler room plan north mechanical room plan detail 'a' fan coil installation detail 'b' terminal unit hydronic coil piping with 3way valve detail 'c' exterior equipment pad adjacent to building detail 'd' heating water piping schematic fan coil schedule fan schedule makeup air unit schedule air cooled packaged chiller schedule gas fired hot water boiler The notes you take as a behavioral health care professional determine the quality of care your patients receive Having notes that are comprehensive yet concise, and informative yet easy for other professionals to use is a skill that often takes years to master Using a predetermined framework in your patient notes can help you improve the quality of your




How To Write Massage Therapy Soap Notes Mblexguide



Soap Notes Dentistry Example
S O A P NOTE S = Subjective or summary statement by the client Usually, this is a direct quote The statement chosen should capture the theme of the session 1 If adding your own explanatory information, place within brackets to make it clear that it is not a direct quoteThe Use of Notes History and Meaning The use of notes or notetaking has long been a method used in early times It has been highly regarded as an important part of human history and development Ancient Greeks kept notes for personal records on different important subjects Note template taking or the use of notes is regarded as a complex human behavior relating to thePromissory note meaning link to How to Make Promissory Note in the Philippines (with Free Sample Templates) How to Make Promissory Note in the Philippines (with Free Sample Templates) Learn how to draft a promissory note through this guide (with accompanying free sample templates) written by a Filipina lawyer Continue Reading About FilipiKnow FilipiKnow is a




Soap Note How To Write Spotless Healthcare Notes Free Template Process Street Checklist Workflow And Sop Software




Soap Note How To Write Spotless Healthcare Notes Free Template Process Street Checklist Workflow And Sop Software
Today, the SOAP note – an acronym for Subjective, Objective, Assessment, and Plan – is the most common method of documentation used by providers to input notes into patients' medical records They allow providers to record and share informationSOAP Method 30 Minute Devotionals With Meaning SOAP Steps 1 Pray (5 minutes) use a list you have prepared 2 Read your Bible (10 minutes) – have a plan 3 Journal using SOAP method (10 minutes) a S = Scripture Write down a meaningful scripture from your reading b O = Observation write 12 paragraph "Observation" about this passage c A = Application Write a 1What does SOAP abbreviation stand for?




Writing Soap Notes Step By Step Examples Templates




Soap Notes Resources Digital Chalkboard
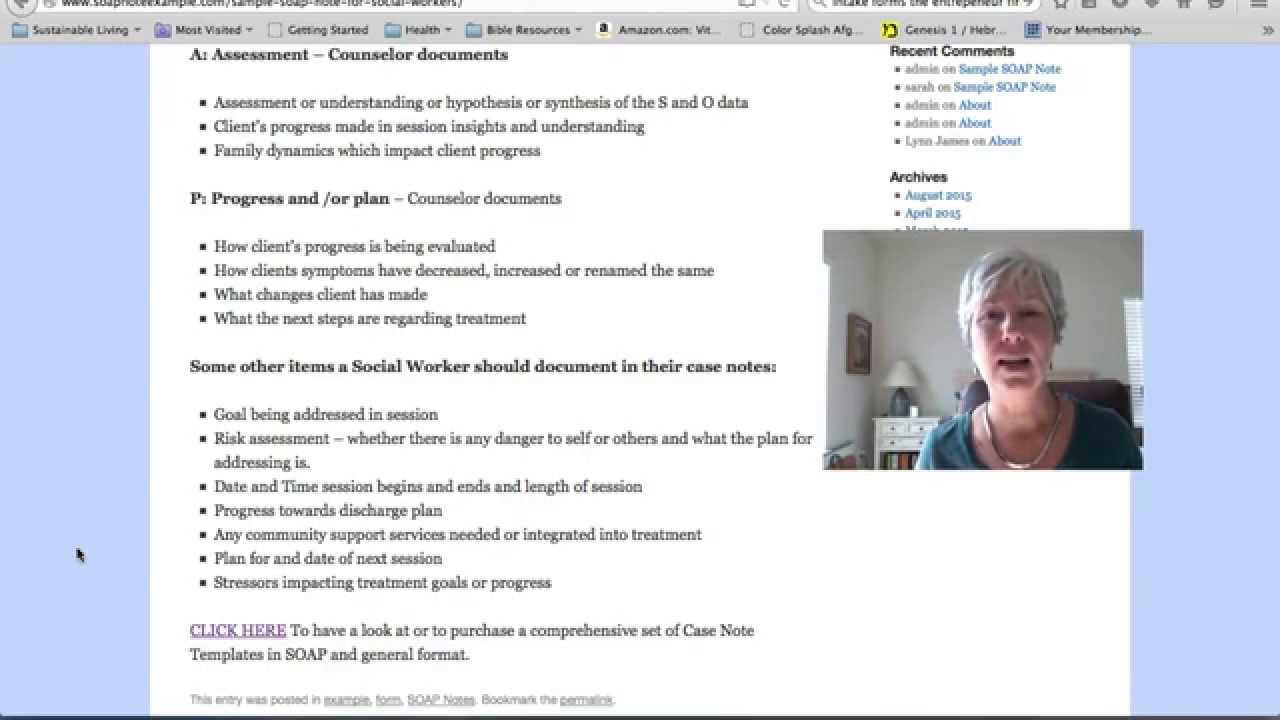
SOAP A chart note usually follows a very simple pattern Subjective (what the patient thinks) = S Objective (what the doctor thinks) = O Assessment (what the diagnosis is) = A Plan (what happens next) = P Not all providers dictate the "SOAP" note format; Sample SOAP Note For Social Workers Whether you are a licensed clinical social worker or an MSW social worker, if you have a case load, chances are you need to write case notes also referred to as progress notes If you are required to write your case notes in SOAP note format this post will give you an example of some of the most importantSummary What Does the Ending Mean?




Tips For Writing Better Mental Health Soap Notes Updated 21




Writing Soap Notes Step By Step Examples Templates
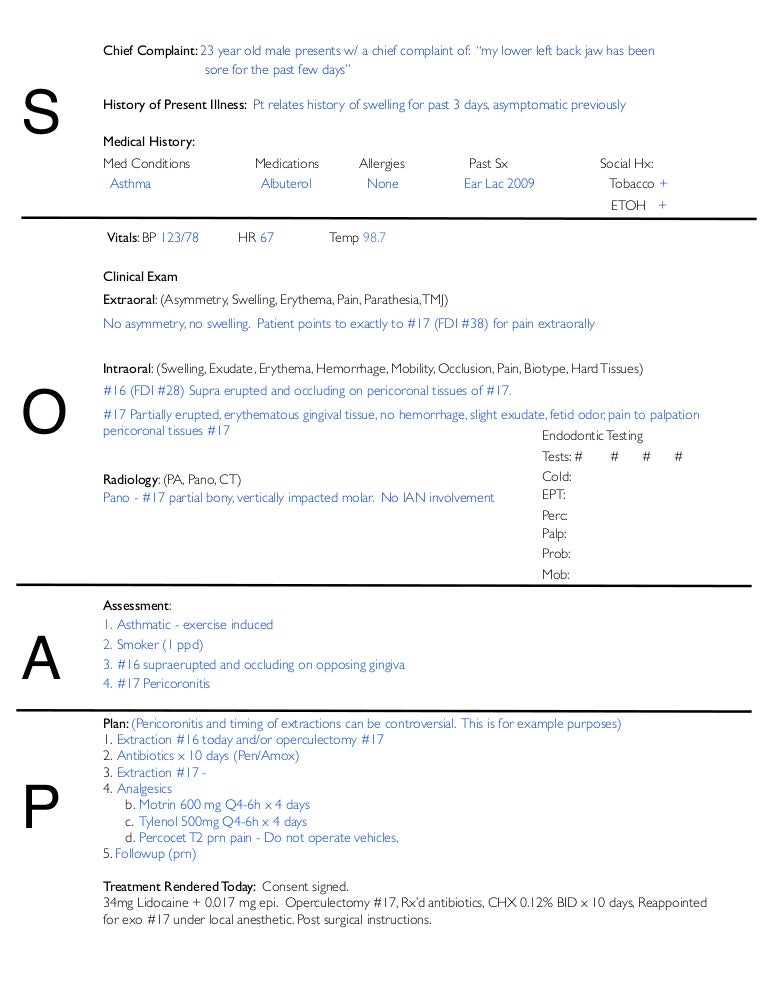
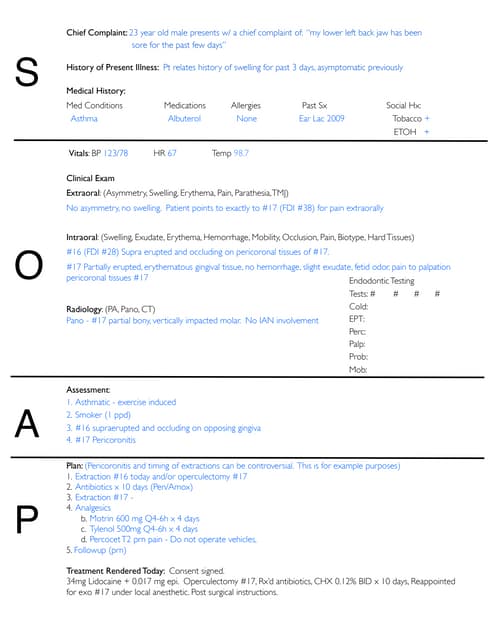
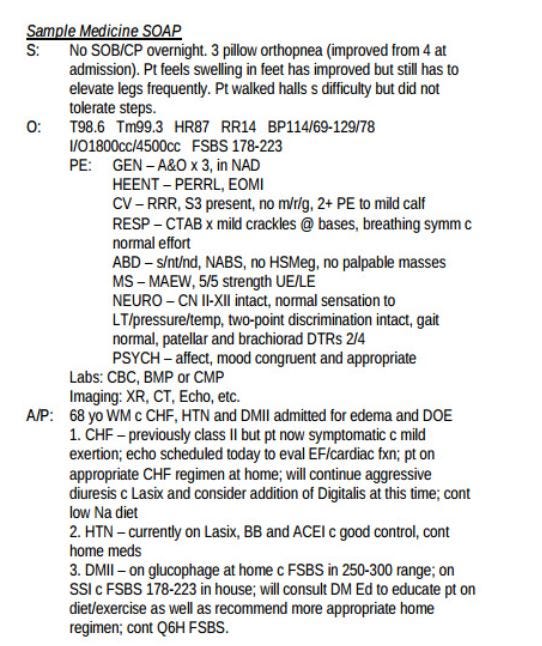
SOAP Notes Dentistry Example 1 Chief Complaint 23 year old male presents w/ a chief complaint of "my lower left back jaw has been sore for the past few days"S History of Present Illness Pt relates history of swelling for past 3 days, asymptomatic previously Medical History Med Conditions Medications Allergies Past Sx Social Hx Asthma Albuterol None Ear Lac 09 The most effective way to study the Bible for beginners is the SOAP method of Bible study What is the SOAP Bible study method In our daily lives, it's important for us to carve out time and prioritize God's word One of my favourite Bible study methods that I was introduced to in University is the SOAP Bible study methodMiami Dade College Medical Center Campus Emergency Medical Technician SSOAP OAP RReport eport FFormatormat (S)ubjective In this area you will document anything that the patient or family & friends tell you



Patient Soap Note Charting Procedures




What Are Soap Notes In Counseling Examples
(Source) A SOAP (s ubjective, o bjective, a ssessment, p lan) note is a method of documentation used specifically by healthcare providers SOAP notes are used so staff can write down critical information concerning a patient in a clear, organized, and quick wayThis is a quick video from the University of Calgary that covers the basics in how to write clinical patient notes It covers some key principles that proteThe Fowler Museum at UCLA, commonly known as The Fowler, and formerly Museum of Cultural History and Fowler Museum of Cultural History, is a museum on the campus of the University of California, Los Angeles (UCLA) which explores art and material culture primarily from Africa, Asia and the Pacific, and the Americas, past and present The Fowler is generally home to three to six



How To Write A Soap Note Occupational Therapy
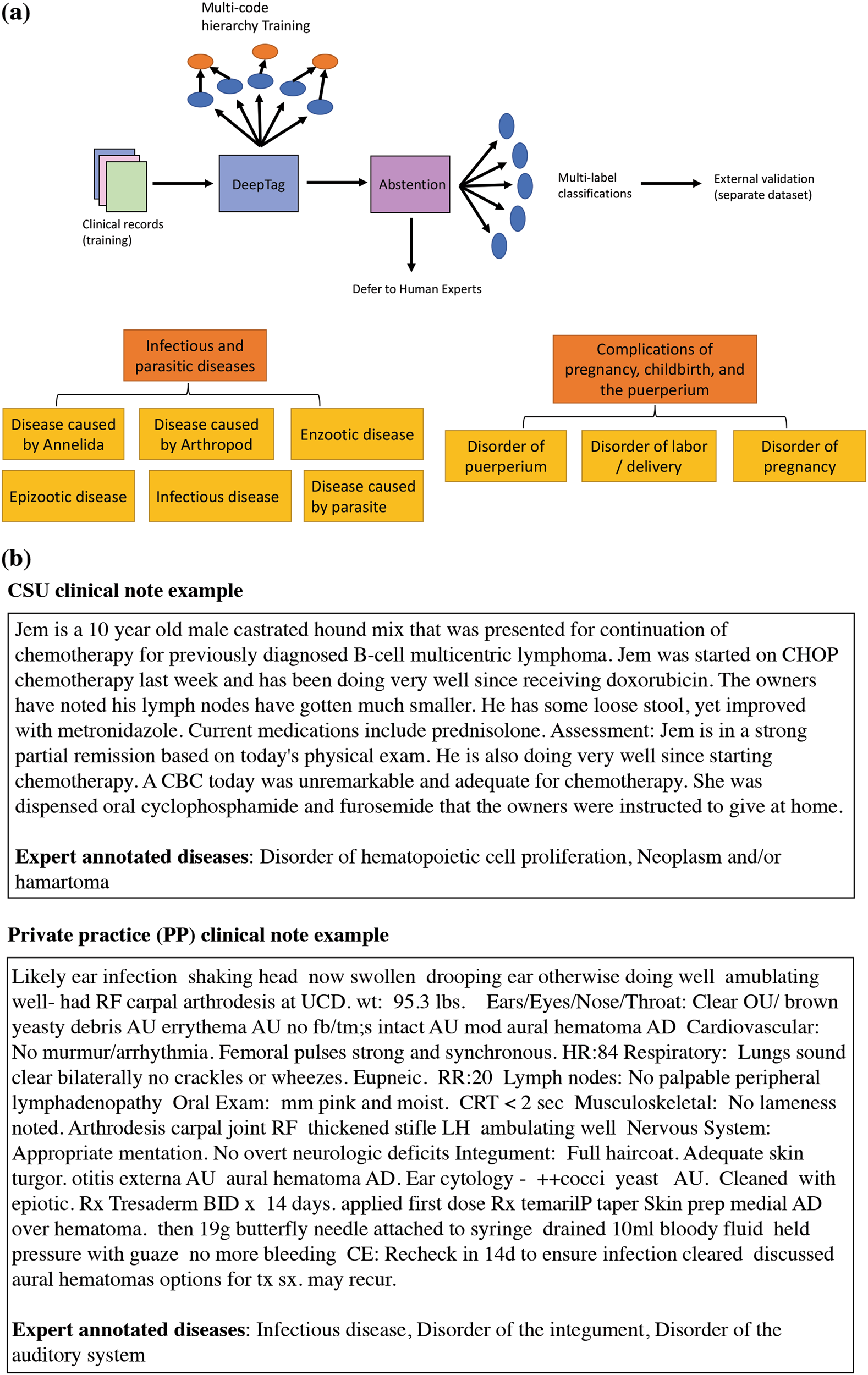



Deeptag Inferring Diagnoses From Veterinary Clinical Notes Npj Digital Medicine
The Subjective section of your soap note is about what the patient is experiencing and how they are handling their concerns Some common examples may include chest pain, decreased appetite, and shortness of breath You can also talk to a family member or spouse to get any necessary informationSOAP Stands for "Simple Object Access Protocol," and can do more than just get your hands clean SOAP is a method of transferring messages, or small amounts of information, over the Internet SOAP messages are formatted in XML and are typically sent using HTTP (hypertext transfer protocol) Both are widely supported data transmissionWriting progress notes SOAPE style SOAPE Subjective The story so far main problems, presumptive diagnosis, tests and treatments;




Free Soap Notes Templates For Busy Healthcare Professionals



Tips For Writing Better Mental Health Soap Notes Updated 21
It stands for "Subjective Objective Assessment Plan," which provides documentation of a patient's condition, diagnosis and treatment SOAP notes were invented in the 1960s by Dr Lawrence Weed of the University of VermontUser Submitted Video What is the cost to diagnose the P2138 CHEVROLET code Labor 10 The cost to diagnose the P2138 CHEVROLET code is 10 hour of labor The auto repair's diagnosis time and labor rates vary by location, vehicle's make and model, and even your engine type Most auto repair shops charge between $75 and $150 per hour HowSometimes they simply state in a narrative way the same information In that case, you would just leave out the abbreviated



Soap Note Made Easy Pt Ot Speech And Nurses Documentation Youtube
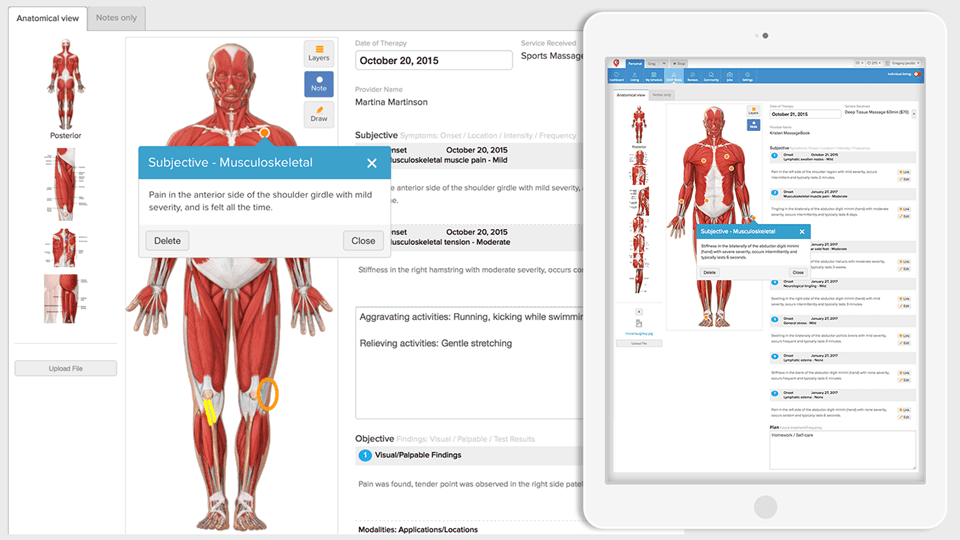



Free Easy To Use Massage Therapy Soap Notes Massagebook Massagebook



40 Fantastic Soap Note Examples Templates ᐅ Templatelab



1




Soap Notes The St John S Pa Program Survival Guide



Progress Notes



40 Fantastic Soap Note Examples Templates ᐅ Templatelab




Soap Wikipedia



Soap Notes Getting Down And Dirty With Medical Translation




What Is Soap Notes The Benefits Of Standardized Notes Cybernet Blog



Tips For Writing Better Mental Health Soap Notes Updated 21




Soap Note Examples Occupational Therapy Quotes Clinical Social Work Soap Note




4 Common Mistakes To Avoid When Writing Soap Notes Simplepractice



Free 14 Blank Note Examples In Pdf Examples




Progress Note Anorexia Nervosa Therapy



Soap Notes Getting Down And Dirty With Medical Translation




Pdf Clinical Note Taking Is Very Challenging For Many Students That Are Novice In The Field Many Times Even Professionals Ask What Type Of Note Taking Is Easy For You So I




Example Of Soap Note Soap Note Medical History Review Of Systems




Examples Of Soap Notes In Nursing Video Lesson Transcript Study Com




Write A Soap Note How To Write A Soap Note



What Are Soap Notes In Counseling Examples



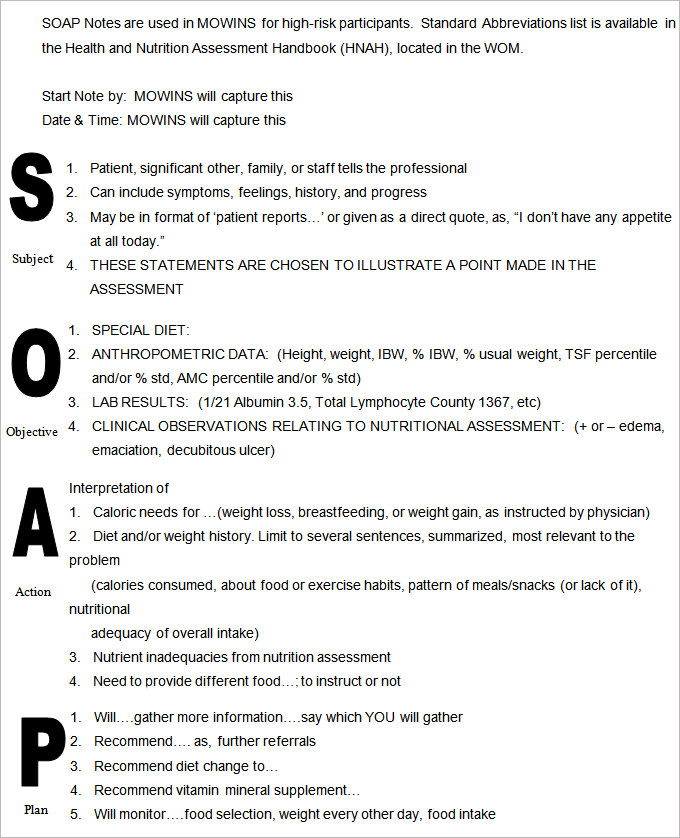
Health Mo Gov Living Families Wic Localagency Wom Pdf Soap Format Pdf



3



Soap Notes Getting Down And Dirty With Medical Translation




How To Write Incredible Physical Therapist Soap Notes



How Soap Notes Paved Way For Modern Medical Documentation




How To Write Massage Therapy Soap Notes Mblexguide




Soap Notes Sample Medicine Soap A P Surgery Soap Pdf Free Download




Aba Practice Daily Simple Guidelines For Writing Soap Notes




Soap Note How To Write Spotless Healthcare Notes Free Template Process Street Checklist Workflow And Sop Software




5 Best Electronic Progress Notes Software For Mental Health Software Advice



Nutritional Progress Notes Ppt Video Online Download




Client Intake Forms Agreements Acuity Scheduling
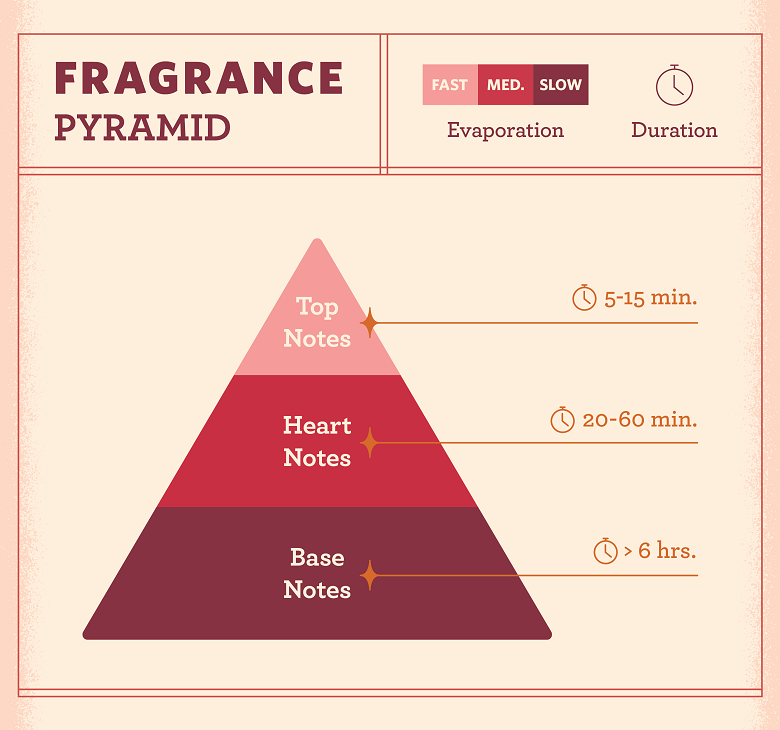



Fragrance Notes Everything You Need To Know Fragrancex




Understanding Soap Format For Clinical Rounds Global Pre Meds



Release Notes What Are They How To Write Them Free Template Included
.png)



Free Massage Soap Notes Forms Massagebook




What Is A Soap Note Jess Brantner Wvu Dietetic Intern




51 Sample Soap Notes In Pdf Ms Word Excel



Free 15 Soap Note Templates In Pdf Ms Word



Soap Notes Getting Down And Dirty With Medical Translation




Quiz Worksheet Soap Notes In Nursing Study Com




Sample Soap Note Template For Counseling Treatment Plan Template Soap Note Clinical Social Work




Documentation Of Pharmaceutical Care Ppt Download




College Certificate Programs Certificateprograms Occupational Therapy Quotes Soap Note Occupational Therapy Activities




4 Common Mistakes To Avoid When Writing Soap Notes Simplepractice




Free Soap Notes Templates For Busy Healthcare Professionals
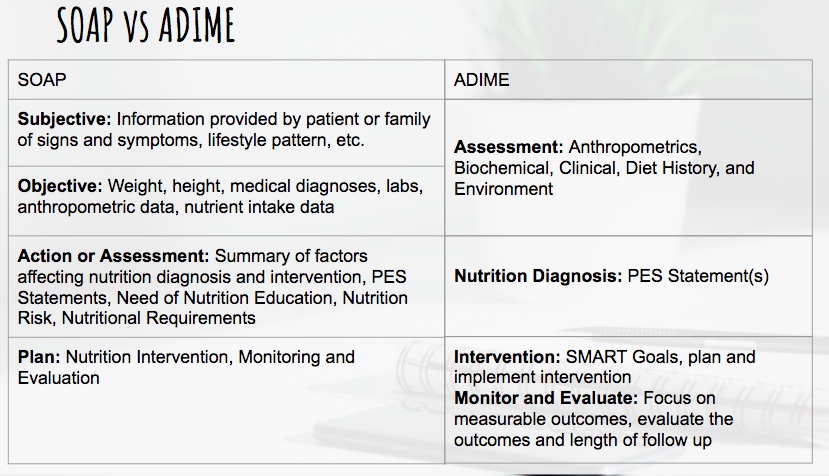



Dietetics Nutritioncare Clinical Documentation 18 Ubc Wiki




Transitioning To Soap 2 0 Webpt Emr Help



1



Free 28 Note Templates Examples In Pdf Doc Examples



Tips For Writing Better Mental Health Soap Notes Updated 21




The Evolution Of Office Notes And The Emr The Caps Note Consult Qd




Practical Guide 10 How To Write Soap Notes The Ot Process



Understanding Clinical Notes This Article By Dot Health Medium
%20for%20veterinary%20practices.jpg)



Soap Format Of Electronic Health Records Emrs For Veterinary Practices




Free Soap Notes Templates For Busy Healthcare Professionals



Implementation Plan What Is It How To Create It Steps Process Bit Blog




Qgbu Joltful4m



Soap Note Writing Tips For Mental Health Counselors Youtube




Free Easy To Use Massage Therapy Soap Notes Massagebook Massagebook




Soap Note



How To Document A Patient Assessment Soap Geeky Medics



Soap Note And Documentation Templates Examples Seniors Flourish




What Are Psychotherapy Notes Vs Progress Notes Theranest




Free Soap Notes Templates For Busy Healthcare Professionals




The Evolution Of Office Notes And The Emr The Caps Note Consult Qd




Crafting The Ideal Ot Note Ot Potential




Free Soap Notes Templates For Busy Healthcare Professionals



Social Workers Easy Way To Write Soap Notes Youtube



1
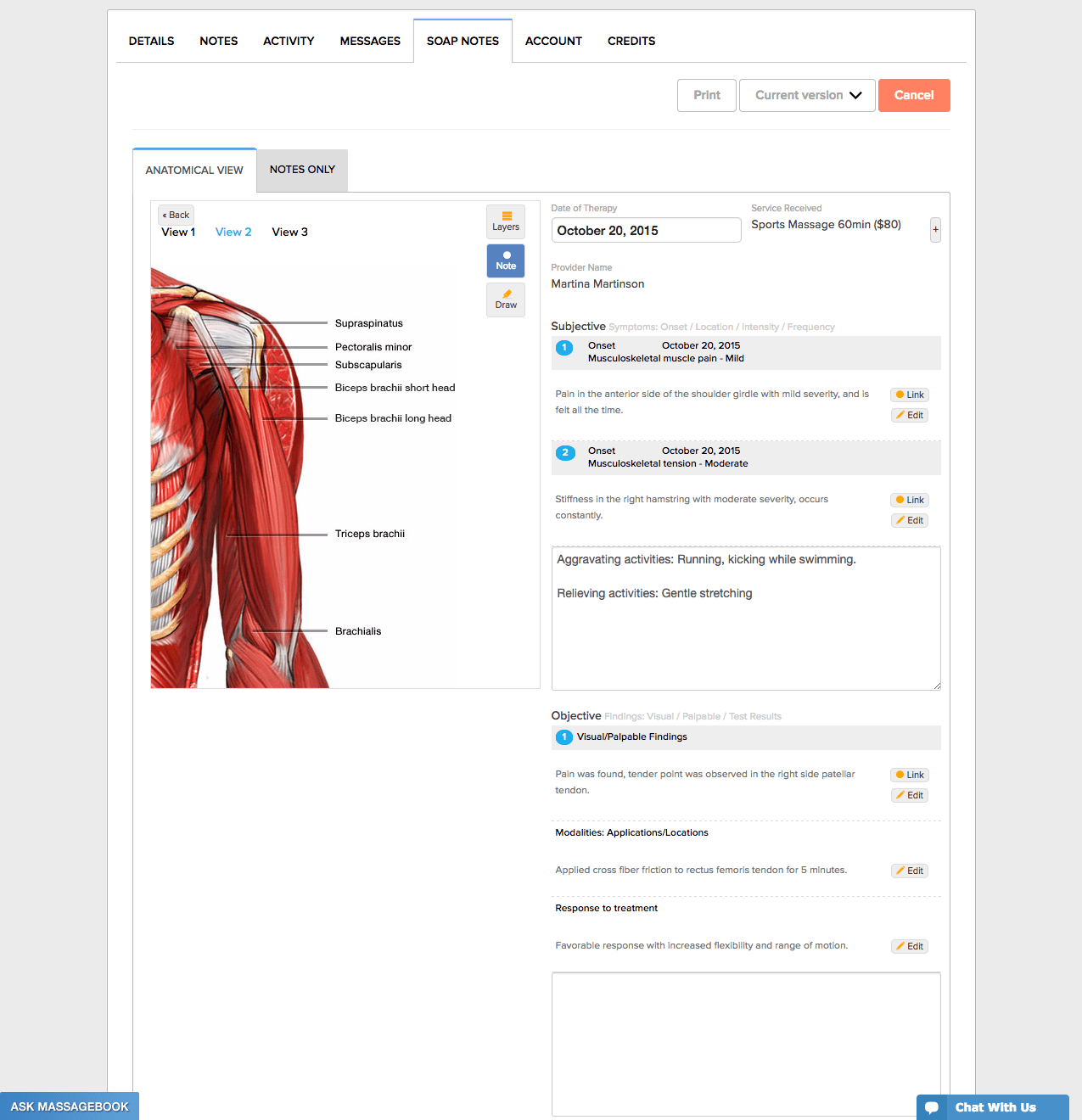



Free Easy To Use Massage Therapy Soap Notes Massagebook Massagebook




Birp Notes A Complete Guide On The Birp Note Taking Format



30 Soap Note Examples Blank Formats Templates



0 件のコメント:
コメントを投稿